Imagine an adult finding it difficult to spread a dosa, or lift a pan to flip an omelet because they can’t move their shoulder. Imagine a child unable to hold a crayon because they have a weak grip. All of these are typical symptoms of injuries to the brachial plexus, a network of nerves that are responsible for controlling the muscles of the shoulder, arm, and hand. These injuries are a result of either Erb’s Palsy or Klumpke’s Palsy.
While both types of palsy can significantly impact the lives of affected individuals, it is important to understand the difference between the two for accurate diagnosis and effective management. This blog will help you understand key differences between Erb’s Palsy and Klumpke’s Palsy. We will also shed light on their unique characteristics, causes, symptoms, and treatment approaches.
You can read more about Brachial Plexus Injury here.
What is Erb’s Palsy?
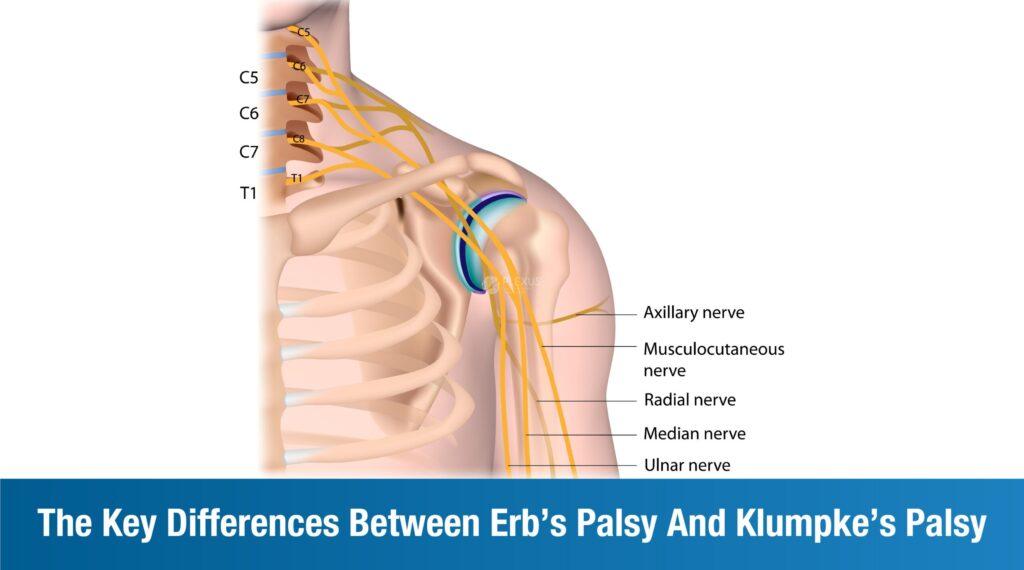
Erb’s Palsy, or Erb-Duchenne palsy, is characterized by weakness of the arm or paralysis due to injury to the brachial plexus. It is typically sustained during childbirth, unfortunately as a result of excessive stretching or pulling of the infant’s neck and/or shoulder while pulling/pushing from the birth canal. Erb’s Palsy specifically affects the C5 and C6 nerve roots of the brachial plexus. The most common causes of Erb’s Palsy are:
- Traumatic childbirth
- Excessive force to baby’s head and neck during delivery
The most common symptoms of Erb’s Palsy include:
- Limited range of motion in affected arm
- Paralysis of the shoulder and upper arm muscles
- Weakness in affected shoulder and arm
- Insufficient muscle control or no sensation in the affected arm
What is Klumpke’s Palsy?
Klumpke’s Palsy, or Dejerine-Klumpke palsy, is a rare type of brachial plexus injury. It affects the C8 and T1 nerve roots, and is characterized by paralysis of the forearm and hand. It is generally sustained due to complications associated with vaginal delivery, such as traumatic delivery, shoulder dystocia (baby’s head passes through the birth canal, but shoulders get stuck behind the mother’s pelvic bone), or baby in breech position. The most common causes of Klumpke’s Palsy are:
- A baby is breech or in any abnormal position in the birth canal
- Improper use of forceps and/or tools during an operative vaginal delivery
- Maternal diabetes
- More than normal maternal weight gain
- High birth weight
- Longer second stage of labour
The most common symptoms of Klumpke’s Palsy are:
- Weakness, numbness, and paralysis in the affected arm and hand
- Poor reflexes
- Stiff joints
- Paralysis
- Sensory loss
- Claw hand, tightened fingers
There have also been cases of associated Horner’s syndrome with specific symptoms such as, ptosis (drooping of the upper eyelid), miosis (constricted pupil), as well as anhidrosis (lack of sweating on one side of the face).
Although rare, there have been instances of Klumpke’s Palsy in adults too. This may be a result of:
- Accidents
- Falls
- Sports injuries
- Trauma to the shoulder area in adults
- Tumors around brachial plexus nerves
Erb’s Palsy and Klumpke’s Palsy – The Fundamental Difference
Since both Erb’s Palsy and Klumpke’s Palsy result from specific complications during the delivery process, they primarily affect newborns and infants. However, the fundamental difference between the two conditions is that Erb’s Palsy affects the upper arm, or upper part of the arm. This includes shoulder, upper bicep, and elbow. Klumpke’s Palsy impacts the lower arm, or lower part of the arm. This includes the forearm, wrist, hand, and fingers.
Treatment Approaches for Erb’s Palsy and Klumpke’s Palsy
To address the unique impact of Erb’s Palsy and Klumpke’s Palsy, Plexus follows a multidisciplinary tailored approach. Our focus is to improve range of motion, muscle strength, as well as overall function of the arm that is affected.
Our first-of-its-kind regenerative rehabilitation program for brachial plexus injury comprises:
- Cell therapy: Mesenchymal Cells (MSCs) help in the repair of torn nerve roots
- Physiotherapy: This involves range of motion exercises, stretching, and strength training
- Occupational therapy: Here, the focus is on fine motor skill development and activities for daily living (ADL) training.
- Splinting and bracing: Although rare, but if a specific demands it, splints and braces are used to maintain alignment, support the affected arm, as well as prevent contractures.
- Patient and caregiver counseling: This includes support services to address the psychological and emotional impact of coping with a brachial plexus injury.
In very rare cases, where there is significant nerve damage, we recommend nerve surgery that involves nerve grafts or transfers to repair damaged nerves and promote healthy nerve function.
FAQs
What is the difference between shoulder dystocia and Erb’s palsy?
Shoulder dystocia refers to difficulties during childbirth when a baby’s head passes through the birth canal. Erb’s Palsy, on the other hand, involves nerve damage. It is a brachial plexus injury often associated with shoulder dystocia which is a complication during delivery. Erb’s Palsy is a specific nerve injury resulting from excessive force applied to the baby’s head and neck during childbirth.
What causes Erb’s palsy?
The main cause of Erb’s Palsy is excessive stretching or tearing of the brachial plexus nerves during childbirth. This typically occurs when there is difficulty delivering the baby’s shoulder, leading to trauma to the brachial plexus.
What is characteristic for Erb’s palsy?
Erb’s Palsy is characterized by weakness or paralysis in the upper part of the arm. It typically affects the muscles controlled by the injured nerves. The most common features of Erb’s Palsy include a limp or paralyzed arm, limited range of motion, and impaired muscle coordination in the affected arm.
Which nerve is damaged in Erb’s palsy?
The C5 and C6 nerve roots are primarily impacted by Erb’s Palsy. These control the muscles of the shoulder, upper arm, and forearm.
How is Erb’s palsy diagnosed?
Erb’s Palsy is often diagnosed through a combination of physical examinations, medical history reviews, and imaging studies like MRIs. Clinical assessments help identify muscle weakness, loss of sensation, and impaired reflexes in the affected arm.










