We are Plexus
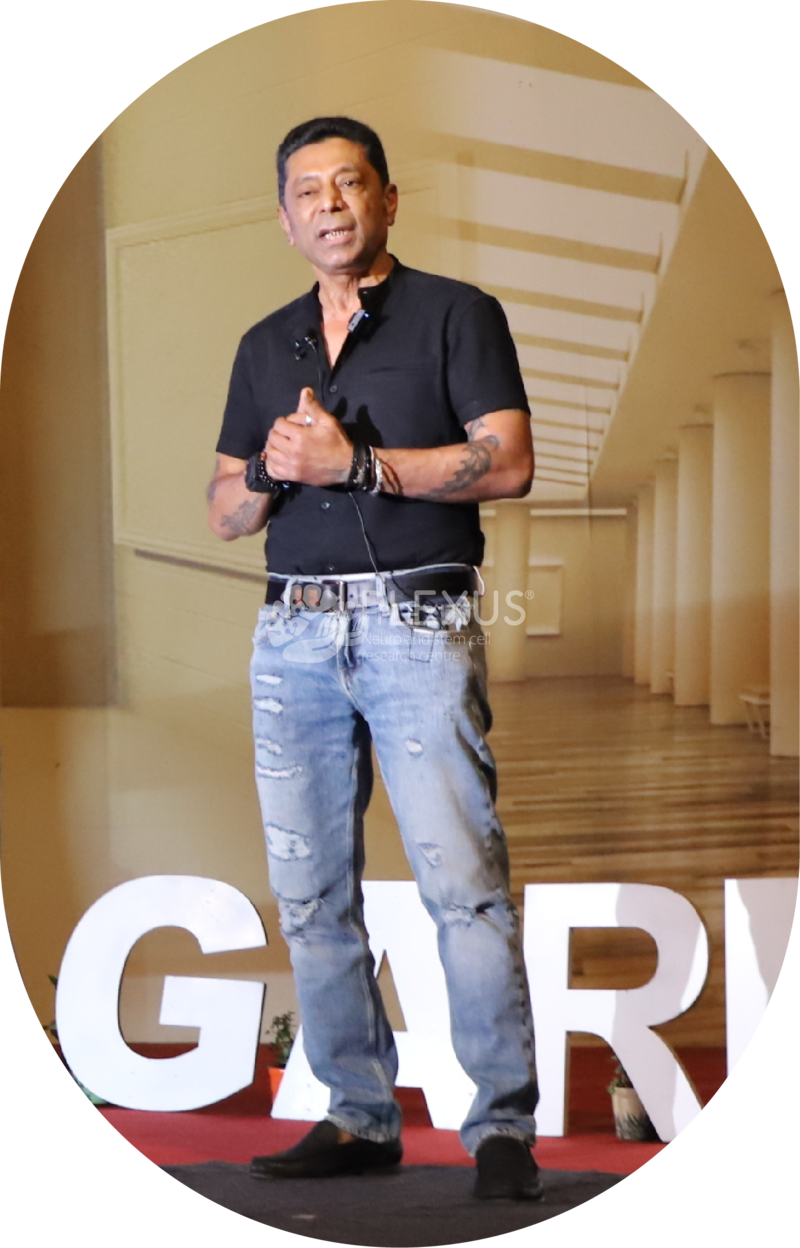
At Plexus Neuro and Stem Cell Research Center, we’re on a mission to transform healthcare worldwide. We offer cutting-edge neurological care that enables patients and their families to envision new possibilities and make progress every day. With world-renowned neurologist Dr Na’eem Sadiq at the helm, we’re proud to be India’s first ISO-certified regenerative rehabilitation and research center. Since 2011, we’ve touched over half a million lives at our Bangalore and Hyderabad centers.